Iodine deficiency and it’s role in hypothyroidism
Iodine deficiency affects more than 1 billion people worldwide and is the leading cause of preventable brain damage¹. Iodine deficiency causes hypothyroidism by decreasing thyroid hormone production. To increase iodine levels, fortification programs have been implemented in a majority of countries through salt iodisation, bread and milk fortification. Goitrogens can block iodine absorption and need to be considered when fortification programs are implemented. Research shows an excess of iodine as well as deficiency can instigate hypothyroidism.
Supplementing iodine at 150ug daily for all adults may decrease iodine deficiency and improve thyroid disease outcomes. However, studies are conflicting and suggest that incorrect levels of iodine supplementation can cause thyroid disease.
Generally, iodine supplementation through food fortification has showed conflicting results in that iodine levels were repleted but with negative adverse effects on thyroid function. Additionally, positive effects on thyroid disease were found in pregnant women with iodised salt, children using iodised oil and pregnant women using supplements.
Iodine supplementation fortified into salt is the most practical and cost-effective avenue of repleting iodine status worldwide and therefore correcting low thyroid function. However, the amount of fortification and correcting the balance of iodine status is conflicting and needs further studies.
Background
Hypothyroidism is an endocrine disorder caused by a deficiency of thyroid hormone. Iodine deficiency is the major cause of hypothyroidism worldwide in iodine deficient areas. In iodine replete areas, Hashimoto’s thyroiditis is the major cause of hypothyroidism, however for this review focus will be on iodine deficiency and excess causing thyroid dysfunction and its role in the management of the disease.
The thyroid gland regulates growth, development and metabolism by using iodine and converting it into triiodothyronine (T3) and thyroxine (T4). Thyroid stimulating hormone (TSH) is produced by the pituitary gland when T3 and T4 levels are low and signals the thyroid to produce more hormone. If iodine levels are too low, even though the gland will compensate for mild to moderate deficiency at the cost of the thyroid being stimulated and enlarged, eventually hormone levels drop and hypothyroidism occurs (1).
In low iodine status, TSH is secreted from the pituitary gland to tell the thyroid to increase the sodium-iodide symporter and absorb more into the thyrocyte. This mechanism will not only absorb more iodide but will reuse iodine more efficiently and reduce renal clearance².
A diet low in iodine can cause an enlarged thyroid gland (goitre) and affect fertility, increase infant mortality and cause mental retardation in offspring called cretinism³. Clinical signs and symptoms of hypothyroidism include fatigue, weight gain, depression, constipation, impaired cognitive function including forgetfulness, cold intolerance, hair loss and menstrual irregularities¹. Groups most at risk are children, pregnant and breastfeeding women and neonates.
Statistics
Iodine status worldwide was deficient for decades until fortification programmes in the 1920’s were put in place predominantly with iodised salt and a small proportion of countries used fortified bread and milk. Since then, in 2014, 112 countries are iodine replete, 29 are deficient and 11 countries have iodine excess¹. Even though Australia has technically an adequate iodine status, 40 % of child bearing women are deficient⁴.
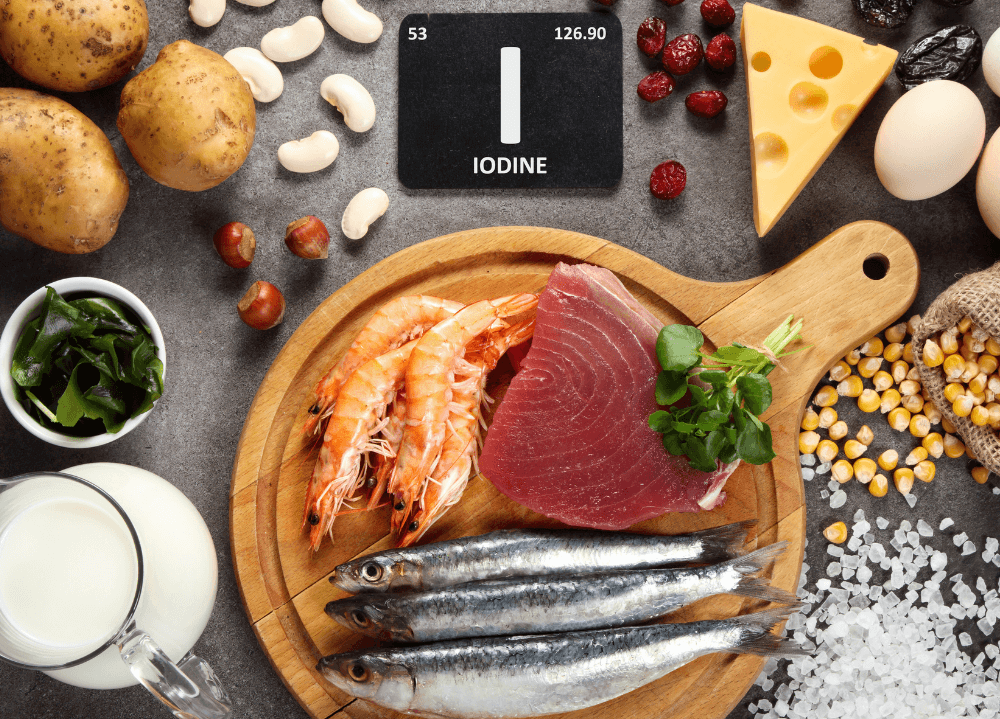
Sources
Iodine is found in the sea and main food sources are seaweed, fish, fortified bread and salt and smaller amounts found in plants dependant on levels in the soil². Salt iodisation has been used throughout the world to control iodine deficiency with great success as it is cost effective and relatively easy to implement. However, there are still countries deficient in iodine causing hypothyroidism including Australia.
Table 1: Approximate iodine content of various foods⁵
Food | Micrograms of iodine per 100g | Micrograms of iodine per serve | Serving size |
Oysters | 160 | 144 | 6 oysters - 90g |
Sushi (containing seaweed) | 92 | 92 | 1 sushi roll - 100g |
Canned salmon | 60 | 63 | 1 small tin - 105g |
Bread (except organic bread) | 46 | 28 | 2 slices bread - 60g |
Steamed snapper | 40 | 50 | 1 fillet - 125g |
Cheddar cheese | 23 | 4 | 2.5cm cube - 16g |
Eggs | 22 | 19 | 2 eggs - 88g |
Ice cream | 21 | 10 | 2 scoops - 48g |
Chocolate milk | 20 | 60 | 1 large glass - 300ml |
Flavoured yoghurt | 16 | 32 | 1 tub - 200g |
Regular milk | 23 | 57 | 1 large glass - 250ml |
Canned tuna | 10 | 10 | 1 small tin - 95g |
Bread (organic) | 3 | 2 | 2 slices - 60g |
Beef, pork, lamb | <1.5 | <1.5 | 2 lamb loin chops |
Apples, oranges, grapes, bananas | <0.5 | <0.6 | 1 apple |
Table 2: Recommended daily intake⁵
RDI for iodine | Micrograms per day |
Younger children (1 to 8 years) | 90 |
Older children (9 to 13 years, boys and girls) | 120 |
Adolescents (14 to 18 years) | 150 |
Men | 150 |
Women | 150 |
Pregnany women | 220 |
Breastfeeding women | 270 |
Table 3: Iodine deficiency table
Deficiency levels | Iodine levels micrograms |
Normal | >100 |
Mild | 50-99 |
Moderate | 20-50 |
Severe | <20 |
Goitrogens
A goitrogen is any substance that interferes with thyroid hormone synthesis. Goitrogens block iodine uptake into the sodium iodide symporter and impair thyroid function only if a person is iodine deficient².
Goitrogens found in the food supply and environment include: thiocyanates from cruciferous vegetables, cassava, smoking cigarettes, halogens found in chlorine, bromine and fluoride, isoflavone phytoestrogens from soy, flavonoids found in quercetin, resveratrol and naringenin, carnitine and medications including lithium². Other sources are nitrates found in drinking water, leafy vegetables, root vegetables and processed meats. The strongest goitrogen is perchlorate, an environmental toxin found in water supplies and cow’s milk².
Excess iodine can also act as a goitrogen, switching off thyroid function as described in the Wollf-Chaikoff effect. The mechanism behind this is from a rat animal study conducted in 1966, Wollf and Chaikoff found that dosing rats with excess iodine produced hypothyroidism⁶. The Wollf Chaikoff effect may only be transient, whereby large intakes of iodine will down regulate the sodium iodide symporter and the thyroid will reduce iodine uptake. This effect is transient and normal iodine absorption will resume 2-3 weeks later⁷. Unfortunately, if there is an underlying thyroid condition such as Grave’s disease, Hashimoto’s thyroiditis, iodine deficiency or any other thyroid dysfunction the sodium iodide symporter may not upregulate and hypothyroidism occurs⁷.
Comparatively, in low iodine status, TSH is secreted from the pituitary gland to tell the thyroid to increase the sodium-iodide symporter and absorb more into the thyrocyte. This mechanism will not only absorb more iodide but will reuse iodine more efficiently and reduce renal clearance².
Iodine fortification
Bread fortification began in Tasmania in 2001 and in Australia nationally in 2009. Iodised salt was included in all bread except organic and bread mixes for home baking⁵.
Data from the national Nutrition Survey reports that women who eat three slices of bread daily are 5 times more likely to reach adequate iodine status and children aged 2-18 are 12 times more likely to be iodine replete⁸.
Current recommendations for iodine levels is 150ug daily and <100ug is deficient. It is considered that since bread fortification in Australia, fortification has corrected iodine deficiency with average levels of 124ug. However, 40.1 % of females aged 16-44 and of child bearing age are still deficient with levels<100ug and 15.8% <50ug⁴. This data suggests Australia’s iodine status may not be adequate and that fortification is not reaching one of the most at risk groups.
An increase in iodine in a deficient area can significantly change thyroid disease positively and negatively¹. In mild to moderate deficient areas research shows an increase in thyroglobulin, increased thyroid volume, development of goitre and thyroid nodules. In moderate to severe iodine deficiency, TSH begins to increase, T4 is declining and there is subclinical hypothyroidism. Once iodine is exhausted chronically with severe deficiency, TSH increases, T3 and T4 decrease, goitre enlarges and overt hypothyroidism occurs¹.
The mechanism of iodine decreasing the occurrence of hypothyroidism, is based on studies that show increasing iodine in deficient areas, normalises thyroid function by decreasing TSH, decreasing thyroid volume and improving T4 levels¹. However, achieving the balance of iodine supplementation is crucial as excess is as detrimental as deficiency.
There is no evidence that measures iodine repletion and hypothyroidism directly, however there is a plethora of studies measuring, T4, TSH, iodine levels, thyroid autoantibodies (TgAb, TPOAb), IQ scores and cognitive function.
Overall, all adults should be given 150ug of iodine per day, whether it be through foods, supplementation or fortified foods. This will ensure that women of childbearing age have sufficient iodine status and decrease the risk of hypothyroidism in pregnancy and in the neonate. 150ug intake daily also decreases the risk of iodine deficiency or excess iodine causing hypothyroidism in adults.
Conclusion
Global deficient iodine levels need to become repleted in order to significantly reduce hypothyroidism caused by iodine deficiency or excess. Iodine deficiency is affected by goitrogens found in food and the environment, as well as excess iodine as described by the Wollf Chaikoff effect.
Studies around the world show that salt iodisation programs in the population and supplements at the individual level have repleted iodine status in 112 countries. However, research shows that hypothyroidism incidence has increased significantly.
Research suggests that the balance of iodine fortification in foods and supplements needs to be high enough to make a difference, but also low enough to decrease adverse effects as well as avoid hypothyroidism. Studies are promising, however more research needs to be conducted on the direct impact of iodine deficiency and the use of iodine to reverse an overt hypothyroid state.
If you are suffering from the effects of iodine deficiency or hypothyroidism, make an appointment today. ALL Naturopath can help enable you to live your best life! Call for an appointment on 0402 926 675.
References
- Zimmermann MB, Boelaert K. Iodine deficiency and thyroid disorders. The Lancet Diabetes & Endocrinology. 2015;3(4):286-95.
- Zimmermann MB, Jooste PL, Pandav CS. Iodine-deficiency disorders. The Lancet. 2008;372(9645):1251-62.
- Pearce EN, Andersson M, Zimmermann MB. Global Iodine Nutrition: Where Do We Stand in 2013? Thyroid. 2013;23(5):523-8.
- ABS. Australian Health Survey: Biomedical Results for Nutrients, 2011-12 , Table 1: Nutrient biomarkers by age and then sex, means and medians Australian Bureau of Statistics. 2011-2012.
- (FSANZ) FSANZ. Iodine in food and Iodine Requirements. 2016.
- Wolff J, Chaikoff IL, Goldberg RC, Meier JR. The Temporary Nature of the Inhibitory action of excess iodide on organic iodine synthesis in the normal thyroid. Endocrinology. 1949;45(5):504-13.
- Koukkou EG, Roupas ND, Markou KB. Effect of excess iodine intake on thyroid on human health. Minerva medica. 2017;108(2):136-46.
- Hynes KL SJ, Otahal P, Reardon MA and Burgess JR. Iodine adequacy in Tasmania sustained after 7 years of mandatory bread fortification The Medical Journal of Australia. 2018;208(3):126.
- Shan Z1 CL, Lian X3, Liu C4, Shi B5, Shi L6, Tong N7, Wang S8, Weng J9, Zhao J10, Teng X1, Yu X1, Lai Y1, Wang W1, Li C1, Mao J1, Li Y1, Fan C1, Teng W1. Iodine Status and Prevalence of Thyroid Disorders After Introduction of Mandatory Universal Salt Iodization for 16 Years in China: A Cross-Sectional Study in 10 Cities. Thyroid: Official Journal of the American Thyroid Association. 2016;26(8):1125-30.
- Sang Z, Chen W, Shen J, Tan L, Zhao N, Liu H, et al. Long-Term Exposure to Excessive Iodine from Water Is Associated with Thyroid Dysfunction in Children. The Journal of Nutrition. 2013;143(12):2038-43.
- Blumenthal N, Byth K, Eastman CJ. Iodine Intake and Thyroid Function in Pregnant Women in a Private Clinical Practice in Northwestern Sydney before Mandatory Fortification of Bread with Iodised Salt. Journal of Thyroid Research. 2012;2012:798963.
- Laurberg P, Cerqueira C, Ovesen L, Rasmussen LB, Perrild H, Andersen S, et al. Iodine intake as a determinant of thyroid disorders in populations. Best Practice & Research Clinical Endocrinology & Metabolism. 2010;24(1):13-27.
- Laurberg P, Jorgensen T, Perrild H, Ovesen L, Knudsen N, Pedersen IB, Rasmussen LB, Carlé A and Vejbjerg P. The Danish investigation on iodine intake and thyroid disease, DanThyr: status and perspectives. The European Journal of Endocrinology. 2006;155:219-28.
- Allan Carlé PL, Inge Bülow Pedersen, Nils Knudsen, Hans Perrild, Lars Ovesen, Lone Banke Rasmussen and Torben Jorgensen. Epidemiology of subtypes of hypothyroidism in Denmark. European Journal of Endocrinology. 2006;154:21-8.
- Krejbjerg A, Bjergved L, Pedersen IB, Knudsen N, Jørgensen T, Perrild H, et al. Thyroid Nodules in an 11-Year DanThyr Follow-Up Study. The Journal of Clinical Endocrinology & Metabolism. 2014;99(12):4749-57.
- Moleti M, Lo Presti VP, Campolo MC, Mattina F, Galletti M, Mandolfino M, et al. Iodine Prophylaxis Using Iodized Salt and Risk of Maternal Thyroid Failure in Conditions of Mild Iodine Deficiency. The Journal of Clinical Endocrinology & Metabolism. 2008;93(7):2616-21.
- Zimmermann MB, Connolly K, Bozo M, Bridson J, Rohner F, Grimci L. Iodine supplementation improves cognition in iodine-deficient schoolchildren in Albania: a randomized, controlled, double-blind study. The American Journal of Clinical Nutrition. 2006;83(1):108-14.
- Glinoer D, De Nayer P, Delange F, Lemone M, Toppet V, Spehl M, et al. A randomized trial for the treatment of mild iodine deficiency during pregnancy: maternal and neonatal effects. The Journal of Clinical Endocrinology & Metabolism. 1995;80(1):258-69.
